In order to establish an accurate diagnosis of the respective etiology and potential complications, detailed information must be obtained on the following topics: a comprehensive clinical history extending as far back as the onset of the diarrheal illness; prior dietary history; breastfeeding history; socioeconomic status and living conditions; prior medical history, including prior infectious diseases and family history. History and physical examination can outline a profile of the patient’s nutritional status and other consequences of the diarrheal illness. The laboratory investigation should include: stool culture and search for ova and parasites in fresh stool specimens, detection of fecal pH and reducing substances search in the stools, search for leukocytes and occult blood in the stools, determination of fecal α1 anti-trypsin and steatocrit.
Considering the high prevalence of carbohydrates intolerance of the diet reported in PD patients as a perpetuating factor of diarrhea, the approach should include overload tests with the various carbohydrates commonly used in the diet, such as lactose, glucose and fructose (Figure 1).
Figure 1- Schematic representation of the physiopathology of lactose malabsorption.
The lactulose load test should also be carried out in order to detect a possible bacterial overgrowth in the small intestine. All these tests should preferably be carried out by the technique of the H2 breath test, because this is a noninvasive method with high sensitivity and specificity (43) (Figure 2).
Figure 2- Lactulose test showing two peaks of H2 production due to bacterial overgrowth in the small bowel.
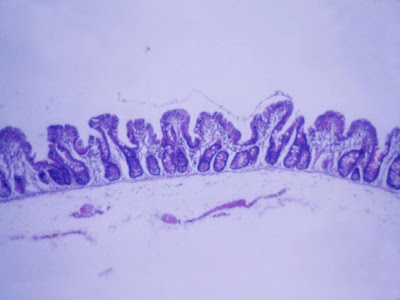
If possible, the determination of fecal electrolytes should also be done, which will distinguish osmotic from secretory diarrhea (44). In many cases, the small bowel biopsy should be performed to evaluate the mucosal architecture and the inflammatory infiltrate in the lamina propria, to investigate specific causes and to demonstrate the extent of the intestinal damage (45) (Figures 3 & 4).
Figure 3- Small bowel biopsy during the period of state of the persistent diarrhea showing subtotal villous athrophy.
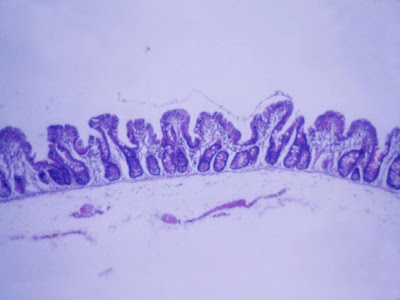 Figure 4- Small bowel biopsy after clinical recovery showing digitiform villi.
Figure 4- Small bowel biopsy after clinical recovery showing digitiform villi.
The knowledge of the intensity and extension of morphological damage enables the appropriate dietary management approach. When concurrent rectal bleeding occurs rectal biopsy should be performed to evaluate the degree and type of inflammation (46) (Figures 5 & 6).
Figure 5- Rectal biopsy showing criptic abscess due to inflammatory process of allergic colitis.
Figure 6- Rectal biopsy with normal structure.
Management
The importance of a proper rehydration and dietary management during the acute diarrheic episode is well known to prevent the progression to PD (47). Antibiotic treatment is only recommended for prolonged infection caused by Salmonella, Giardia, Cyclospora and enteroaggregative Escherichia coli strains (the latter especially if the infant is less than 3 months old or malnourished, immunosuppressed or with signs of systemic disease) (48) and in the presence of bloody diarrhea when Shigella is isolated in the stools (49). The decision of prescribing antibiotics is limited to laboratory evidence of the enteropathogen and type of microbial resistance (50,51).
The use of an extensive hydrolyzed protein formula or even a mixture of amino acids based formula is indicated in the following clinical circumstances: 1- acute diarrhea in infants under six months or less than one year of age with severe malnutrition, associated with dehydration and/or metabolic disorders; 2- PD with aggravation of the nutritional status or frequent recurrence of dehydration and/or metabolic acidosis (52) (Figures 7 & 8).
Figure 7- Our patient during the clinical recovery process.
Figure 8- Our patient completely recovery from the Escherichia coli infection.
The prescription of zinc and vitamin A seems to have a positive impact over the cellular immune system, helping in the treatment of acute and persistent diarrhea (53,54,55). It is necessary to prescribe a daily supplementation of zinc at a dose of 10 mg/day for a period of 2 to 3 months after the diarrhea episode has ceased.
Prophylaxis
In conclusion, UNICEF and WHO propose seven strategic measures to be implemented around the world for diarrheal diseases control, namely: 1- Fluid replacement to prevent dehydration, 2- Zinc treatments, which decrease the severity and duration of the attack, 3- Immunization against rotavirus and measles, 4- Early and exclusive breastfeeding and vitamin A supplementation, 5- Hand washing with soap, 6- Improved water supply quantity and quality, including safe storage of water in homes, 7- Promoting community-wide sanitation (11). Other proposals for reducing the incidence of PD include prolonged and exclusive breastfeeding and strategies to ensure safe food supply for adequate weight and height development considering that the protein-energy malnutrition is a risk factor for this syndrome (11). Gut infections lead to malnutrition and malnutrition increases the risk for further intestinal infections. Ceasing the vicious cycle of diarrhea-malnutrition should be the priority goal for Pediatricians for a safe development of children (44).
Considering the high prevalence of carbohydrates intolerance of the diet reported in PD patients as a perpetuating factor of diarrhea, the approach should include overload tests with the various carbohydrates commonly used in the diet, such as lactose, glucose and fructose (Figure 1).
Figure 1- Schematic representation of the physiopathology of lactose malabsorption.
The lactulose load test should also be carried out in order to detect a possible bacterial overgrowth in the small intestine. All these tests should preferably be carried out by the technique of the H2 breath test, because this is a noninvasive method with high sensitivity and specificity (43) (Figure 2).
Figure 2- Lactulose test showing two peaks of H2 production due to bacterial overgrowth in the small bowel.
If possible, the determination of fecal electrolytes should also be done, which will distinguish osmotic from secretory diarrhea (44). In many cases, the small bowel biopsy should be performed to evaluate the mucosal architecture and the inflammatory infiltrate in the lamina propria, to investigate specific causes and to demonstrate the extent of the intestinal damage (45) (Figures 3 & 4).
Figure 3- Small bowel biopsy during the period of state of the persistent diarrhea showing subtotal villous athrophy.
The knowledge of the intensity and extension of morphological damage enables the appropriate dietary management approach. When concurrent rectal bleeding occurs rectal biopsy should be performed to evaluate the degree and type of inflammation (46) (Figures 5 & 6).
Figure 5- Rectal biopsy showing criptic abscess due to inflammatory process of allergic colitis.
Figure 6- Rectal biopsy with normal structure.
Management
The importance of a proper rehydration and dietary management during the acute diarrheic episode is well known to prevent the progression to PD (47). Antibiotic treatment is only recommended for prolonged infection caused by Salmonella, Giardia, Cyclospora and enteroaggregative Escherichia coli strains (the latter especially if the infant is less than 3 months old or malnourished, immunosuppressed or with signs of systemic disease) (48) and in the presence of bloody diarrhea when Shigella is isolated in the stools (49). The decision of prescribing antibiotics is limited to laboratory evidence of the enteropathogen and type of microbial resistance (50,51).
The use of an extensive hydrolyzed protein formula or even a mixture of amino acids based formula is indicated in the following clinical circumstances: 1- acute diarrhea in infants under six months or less than one year of age with severe malnutrition, associated with dehydration and/or metabolic disorders; 2- PD with aggravation of the nutritional status or frequent recurrence of dehydration and/or metabolic acidosis (52) (Figures 7 & 8).
Figure 7- Our patient during the clinical recovery process.
Figure 8- Our patient completely recovery from the Escherichia coli infection.
The prescription of zinc and vitamin A seems to have a positive impact over the cellular immune system, helping in the treatment of acute and persistent diarrhea (53,54,55). It is necessary to prescribe a daily supplementation of zinc at a dose of 10 mg/day for a period of 2 to 3 months after the diarrhea episode has ceased.
Prophylaxis
In conclusion, UNICEF and WHO propose seven strategic measures to be implemented around the world for diarrheal diseases control, namely: 1- Fluid replacement to prevent dehydration, 2- Zinc treatments, which decrease the severity and duration of the attack, 3- Immunization against rotavirus and measles, 4- Early and exclusive breastfeeding and vitamin A supplementation, 5- Hand washing with soap, 6- Improved water supply quantity and quality, including safe storage of water in homes, 7- Promoting community-wide sanitation (11). Other proposals for reducing the incidence of PD include prolonged and exclusive breastfeeding and strategies to ensure safe food supply for adequate weight and height development considering that the protein-energy malnutrition is a risk factor for this syndrome (11). Gut infections lead to malnutrition and malnutrition increases the risk for further intestinal infections. Ceasing the vicious cycle of diarrhea-malnutrition should be the priority goal for Pediatricians for a safe development of children (44).

References
43- Eisemann A, Amann A, Said M, Datta B, Ledochovsky M. Implementation and interpretation of hydrogen breathe tests. J Breath Res 2008; 2:1-9.
44- Schiller LR. Chronic diarrhea. Curr Treat Options Gastroenterol 2005; 8:259-66.
45- Serra S, Jani PA. An aprproach to duodenal biopsies. J Clin Pathol 2006; 59:1133-50.
46- Silva JGN, Brito T, Damião AOMC, Laudanna AA, Sipahi AM. Histologic study of colonic mucosa in patients with chronic diarrhea and normal colonoscopic findings. J Clin Gastroenterol 2006; 40: 44-8.
47- Lins MGM, Mota MEFA, Silva GAP. Fatores de risco para diárreia persistente em lactentes. Arq. Gastroenterol 2003; 40: 239-246.
49- World Health Organization. Handbook IMCI: Integrated Management of Childhood llness. Geneva: WHO/UNICEF; 2006.http://whqlibdoc.who.int/publications/2005/9241546441.pdf.
50- Amadi B, Mwiya M, Musuku J, Watuka A, Sianong S, Ayoub A et al. Effect of nitazoxanide on morbidity and mortality in Zambian children with cryptosporidiosis: a randomised controlled trial. Lancet 2002; 360:1375-80.
51- Adagu IS, Nolder D, Warhurst DC, Rossignol JF. In vitro activity of nitazoxanide and related compounds against isolates of Giardia intestinalis, Entamoeba histolytica and Trichomonas vaginalis. J Antimicrob Chemother 2002; 49:103-11.
52- Oliva CAG, Palma D. Suporte nutricional nas diarréias aguda e persistente In: Barbieri D, Palma D. Gastroenterologia e Nutrição, São Paulo: Atheneu; 2001: 259-69.
53- Strand TO, Chandyo RK, Bahl R, Sharma PR, Adhikari RK, Bhandari N et al. Effectiveness and Efficacy of Zinc for the Treatment of Acute Diarrhea in Young Children. Pediatrics 2002; 109:898-903.
54- Lukacik M, Thomas RL, Aranda JV. A meta-analysis of the effects of oral zinc in the treatment of acute and persistent diarrhea. Pediatrics 2008;121:326-36.
55- RobberstadI B, Strand T; Black RE; Sommerfelt H. Cost-effectiveness of zinc as adjunct therapy for acute childhood diarrhoea in developing countries. Bull WHO; 82 Geneva July 2004







Nenhum comentário:
Postar um comentário